
Wikipedia:WikiProject_Medicine/Translation_task_force/RTT/Low_back_pain

{{Infobox symptom
| Name = 下背痛
| Image = Lumbar region in human skeleton.svg
| Caption = 下背痛是種常見而所費不貲的病痛
| DiseasesDB =
| ICD10 = {{ICD10|M|54|5|m|50}}
| ICD9 = {{ICD9|724.2}}
| ICDO =
| OMIM =
| MedlinePlus = 007422
| MedlinePlus_mult = {{MedlinePlus2|007425}}
| eMedicineSubj = pmr
| eMedicineTopic = 73
| MeshID = D017116
}}
Low back pain or lumbago /lʌmˈbeɪɡoʊ/ is a common disorder involving the muscles and bones of the back. It affects about 40% of people at some point in their lives. Low back pain (often abbreviated as LBP) may be classified by duration as acute (pain lasting less than 6 weeks), sub-chronic (6 to 12 weeks), or chronic (more than 12 weeks). The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain.
’’’下背痛’’’({{lang-en|[[:en:low back pain|low back pain]],有時簡稱為[[:en:LBP|LBP]]或稱[[:en:lunbago|lunbago]],/lʌmˈbeɪɡoʊ/}})也有不少人稱之為「腰痛」[譯注1],是一種常見的背部{{link-en|肌肉骨骼傷病|Musculoskeletal disorder}}。該疾病影響了許多民眾的生活。下背痛可依[[疼痛]]時間長度,分為急性(小於6週)、亞慢性(6至12週)與慢性(大於12週)。依照下背痛的發生原因,可以更進一步分為機械痛、非機械痛與{{link-en|轉移痛|Referred pain}}。
<!--Cause and diagnosis -->
In most episodes of low back pain, a specific underlying cause is not identified or even looked for, with the pain believed to be due to mechanical problems such as muscle or joint strain. If the pain does not go away with conservative treatment or if it is accompanied by "red flags" such as unexplained weight loss, fever, or significant problems with feeling or movement, further testing may be needed to look for a serious underlying problem. In most cases, imaging tools such as X-ray computed tomography are not useful and carry their own risks. Despite this, the use of imaging in low back pain has increased. Some low back pain is caused by damaged intervertebral discs, and the straight leg raise test is useful to identify this cause. In those with chronic pain, the pain processing system may malfunction, causing large amounts of pain in response to non-serious events.
<!-- 成因與診斷 -->
幾乎所有的下背痛,多無法找到或辨別其病源;而這類的下背痛成因,推測肇因為機械問題,例如{{link-en|扭傷|Strain (injury)}}或{{link-en|挫傷|Sprain}}。如果下背痛在保守療法後仍無法止痛,或者伴隨一些「{{link-en|危險徵象|Red_flag#Science}}」如不明原因的體重減輕、發燒,抑是在行動或感覺上有明顯異狀,則需進一步檢查是否有較嚴重的潛在問題。在多數情況下,如[[X射線電腦斷層掃描]]一類的影像檢查用處不大,而且檢查本身具有風險;儘管如此,對下背痛使用影像檢查檢驗仍屬常見。部分下背痛則起因於[[椎間盤]]的損傷,而{{link-en|舉腿試驗|Straight leg raise}}是檢查椎間盤損傷的有效辨別方式。對慢性下背痛而言,有時疼痛處理系統會失常,造成在輕度刺激下,疼痛反應劇烈。
<!-- Treatment -->
The treatment of acute nonspecific low back pain is typically with conservative measures such as the use of simple pain medications and the continuation of as much normal activity as the pain allows. Medications are recommended for the duration that they are helpful, withacetaminophen (also known as paracetamol) as the preferred first medication. The symptoms of low back pain usually improve within a few weeks from the time they start, with 40-90% of people completely better by six weeks.
<!-- 治療 -->
針對急性發作且未有明確病因的下背痛,一般採「保守治療」的方式─使用{{link-en|鎮痛藥|Analgesic}}減緩疼痛,以及在可忍耐的疼痛下繼續進行日常行為。止痛藥一般以{{link-en|對乙醯氨基酚|acetaminophen}}為第一線用藥,多使用到症狀改善為止。下背痛的症狀通常在使用藥物數週後改善,大約有40-90%的人六週後明顯改善。
A number of other options are available for those who do not improve with usual treatment. Opioids may be useful if simple pain medications are not enough, but they are not generally recommended due to side effects. Surgery may be beneficial for those with disc-related chronic pain and disability. It may also be useful for those with spinal stenosis. No clear benefit has been found for other cases of non-specific low back pain. Low back pain often affects mood, which may be improved by counseling and/or antidepressants. Additionally, there are many alternative medicine therapies, including the Alexander technique and herbal remedies, but there is insufficient evidence to recommend them confidently. The evidence for chiropractic care and spinal manipulation is mixed.
對於使用正常療法後仍無法改善下背痛的患者,會選擇其他治療方法。如果簡單的止痛藥無法解除疼痛,[[鴉片類藥物]]可能有幫助,但通常會因[[鴉片類藥物]]的副作用而不建議使用。對於因椎間盤相關的慢性疼痛與失能者,手術是有效的解決方法。手術也可能對{{link-en|脊椎狹窄症候群|Spinal stenosis}}引發的疼痛有效,但對於其他非特定原因的下背痛,則無法證實手術是否有效。下背痛通常會影響患者的情緒,這可以藉由[[心理治療]]或[[抗憂鬱劑]]改善。此外,還有許多[[替代醫學]]療法,包含[[亞歷山大技巧]]與[[草藥醫學]],但這些療法無足夠證據能佐證其療效。實驗證實,使用[[脊骨神經醫學]]照護與{{link-en|脊椎矯正|Spinal manipulation}}治療下背痛的療效,目前是好壞參半。
原始條目內容 (未整合)
下背痛,顧名思義就是指下背部的疼痛,通常是指背部肋骨下緣以下的部分,由於好發於第四和第五腰椎或第五腰椎和第一薦椎間,是現代人主要的文明病之一。
與下背痛相對應的一組詞彙是lower back pain;
In the common presentation of acute low back pain, pain develops after movements that involve lifting, twisting, or forward-bending. The symptoms may start soon after the movements or upon waking up the following morning. The description of the symptoms may range from tenderness at a particular point to diffuse pain. It may or may not worsen with certain movements, such as raising a leg, or positions, such as sitting or standing. Pain radiating down the legs (known as sciatica) may be present. The first experience of acute low back pain is typically between the ages of 20 and 40. This is often a person’s first reason to see a medical professional as an adult.[1] Recurrent episodes occur in more than half of people[2] with the repeated episodes being generally more painful than the first.[1]
急性下背痛常於舉重物、扭腰、前彎腰之後發生;在移動或清晨起床剛坐起身時,症狀可能會瞬間加劇。至於像抬腿、站著或坐下等動作,則不一定會引起疼痛。疼痛有可能只侷限在特定的壓痛點,也可能是大範圍的疼痛;此外,疼痛可能從下背部往腿部放射性延伸(泛稱為"{{link-en|坐骨神經痛|Sciatica}}")。初次發生下背痛的年齡,多是在20到40歲之間,這也是成人最常見的求診原因[1]。五成以上的下背痛患者,在好轉後仍會復發[2],且復發後的疼痛情形,通常比初次發生時更嚴重[1]。
Other problems may occur along with low back pain. Chronic low back pain is associated with sleep problems, including a greater amount of time needed to fall asleep, disturbances during sleep, a shorter duration of sleep, and less satisfaction with sleep.[3] In addition, a majority of those with chronic low back pain show symptoms of depression[4] or anxiety.[5]
下背痛常和其他身體症狀一起發生。慢性下背痛經常伴隨睡眠問題,例如入睡時間增長、睡眠中斷、睡眠時間變短、睡眠品質不佳等[3]。此外,許多慢性下背痛的病人合併有[[憂鬱]][4]及[[焦慮]][5]的症狀。

[[File:Lagehernia.png|thumb|A herniated disc as seen on MRI, one possible cause of low back pain.]]
[[File:Lagehernia.png|thumb|磁振造影中可觀察到椎間盤突出,此為下背痛可能的原因之一。]]
Low back pain is not a specific disease but rather a complaint that may be caused by a large number of underlying problems of varying levels of seriousness.[6]The majority of LBP does not have a clear cause[1] but is believed to be the result of non-serious muscle or skeletal issues such as sprains or strains.[7] Obesity, smoking, weight gain during pregnancy, stress, poor physical condition, poor posture, and poor sleeping position may also contribute to low back pain.[7] A full list of possible causes includes many less common conditions.[8] Physical causes may include osteoarthritis, rheumatoid arthritis, degeneration of the discs between the vertebrae or a spinal disc herniation, a broken vertebrae (such as from osteoporosis) or, rarely, an infection or tumor of the spine.[9]
下背痛並非單一的疾病,而是由多重原因引起的症狀[6]。大部分的下背痛找不到明確病因[1],但絕大多數和肌肉{{link-en|拉傷|Strain (injury)}}、{{link-en|扭傷|sprain}}有關[7]。肥胖、抽菸、懷孕時體重增加、壓力、身體狀況不佳、姿勢不良、睡姿不良等,也可能造成下背痛[7]。此外,可能引起{{link-en|下背痛的原因|Differential diagnosis|鑒別診斷}}可列出一長串[8],包括{{link-en|骨關節炎|osteoarthritis}}、{{link-en|類風濕性關節炎|rheumatoid arthritis}}、脊椎{{link-en|椎間盤退化|degeneration of the discs}}、脊椎{{link-en|椎間盤突出|spinal disc herniation}}、{{link-en|脊椎壓迫性骨折|vertebral compression fracture}}(常見於{{link-en|骨質疏鬆|osteoporosis}});而脊椎感染或腫瘤也可能導致下背痛,但並不常見[9]。
Women may have acute low back pain from medical conditions affecting the female reproductive system, including endometriosis, ovarian cysts, ovarian cancer, or uterine fibroids.[10] Nearly half of all pregnant women report pain in the lower back or sacral area during pregnancy, due to changes in their posture and center of gravity causing muscle and ligament strain.[11]
婦女的生殖系統相關疾病,可能與婦女下背痛有關,包括{{link-en|子宮內膜異位症|endometriosis}}、{{link-en|卵巢囊腫|ovarian cysts}}、{{link-en|子宮肌瘤|uterine fibroids}}等[10]。約有一半的懷孕婦女,有下背痛或[[骶骨|尾椎區域]]疼痛的情況;原因可能為懷孕時的姿勢改變及重心轉移,造成肌肉或韌帶拉傷,因而引發疼痛[11]。
背部解剖 Back structures

The five lumbar vertebrae define the lower back region
下背區域指圖中深黃色處「Lumbar curve」的五節腰椎之範圍

The structures surrounding and supporting the vertebrae can be sources of low back pain
下背痛可能源自所有支撐脊椎骨以及脊椎骨附近的身體結構。
|The lumbar region in regards to the rest of the spine.|The nerve and bone components of the vertebrae.
{{double image|right|Illu vertebral column.jpg|200|ACDF oblique annotated english.svg|200|下背區域指圖中深黃色處「Lumbar curve」的五節腰椎之範圍。|下背痛可能源自所有支撐脊椎骨以及脊椎骨附近的身體結構。|The lumbar region in regards to the rest of the spine |The nerve and bone components of the vertebrae}}
The lumbar (or lower back) region is made up of five vertebrae (L1-L5). In between these vertebrae are fibrocartilaginous discs, which act as cushions, preventing the vertebrae from rubbing together while at the same time protecting the spinal cord. Nerves come from and go to the spinal cord through specific openings between the vertebrae, providing the skin with sensations and messages to muscles. Stability of the spine is provided by the ligaments and muscles of the back and abdomen. Small joints called facet joints limit and direct the motion of the spine.[12]
所謂的下背({{lang-en|[[:en:lumbar|lumbar]]或[[:en:lower back|lower back]]}})是指由[[椎骨切迹|腰椎]]第一節到第五節所組成的區域。在每節腰椎中間會有{{link-en|纖維軟骨|Fibrocartilage}}所構成的{{link-en|椎間盤|Intervertebral_disc}},這些椎間盤具有「彈性墊」的作用,可防止脊椎之間直接相互摩擦而傷害到[[脊髓]]。脊髓延伸出的脊神經從{{link-en|脊椎側面的開孔|Intervertebral_foramina|椎間孔}}穿出,支配身體的肌肉、同時也傳送體表的感覺至中樞神經系統。脊椎的穩定主要靠背部和腹部的肌肉及韌帶來提供。每節脊椎的相接處,有所謂的「{{link-en|小面關節/關節突間關節|Zygapophysial_joint}}」,會限制及導向脊椎的運動[12]。
The multifidus muscles run up and down along the back of the spine, and are important for keeping the spine straight and stable during many common movements such as sitting, walking and lifting.[13] A problem with these muscles is often found in someone with chronic low back pain, because the back pain causes the person to use the back muscles improperly in trying to avoid the pain.[14] The problem with the multifidus muscles continues even after the pain goes away, and is probably an important reason why the pain comes back.[14] Teaching people with chronic low back pain how to use these muscles is recommended as part of a recovery program.[14]
脊椎旁有一組稱作{{link-en|多裂肌群|multifidus muscles}}的肌肉,縱向連接著每節脊椎,使脊椎在做許多動作如坐下、行走、舉起物品時能維持垂直及穩定[13]。慢性背痛的病人為了避免疼痛,常會擺出不正確的姿勢[14],因而也使多裂肌群不正常而長時間的收縮或伸張。這樣的狀況在背痛消失後仍有可能持續存在,因此也可能是造成慢性背痛的病人疼痛復發的重要原因之一[14]。教導慢性背痛的病人如何正確地使用多裂肌群被建議列入復建計畫之中[14]。
An intervertebral disc has a gelatinous core surrounded by a fibrous ring.[15]When in its normal, uninjured state, most of the disc is not served by either the circulatory or nervous systems – blood and nerves only run to the outside of the disc.[15] Specialized cells that can survive without direct blood supply are in the inside of the disc.[15] Over time, the discs lose flexibility and the ability to absorb physical forces.[6] This decreased ability to handle physical forces increases stresses on other parts of the spine, causing the ligaments of the spine to thicken and bony growths to develop on the vertebrae.[6] As a result, there is less space through which the spinal cord and nerve roots may pass.[6] When a disc degenerates as a result of injury or disease, the makeup of a disc changes: blood vessels and nerves may grow into its interior and/or herniated disc material can push directly on a nerve root.[15] Any of these changes may result in back pain.[15]
椎間盤的組成為凝膠狀的核心({{lang-en|[[:en:Nucleus pulposus|gelatinous core]]}})及環繞包覆在椎間盤外側的纖維環({{lang-en|[[:en:Annulus fibrosus disci intervertebralis|fibrous ring]]}})[15]。正常情況下,[[循環系統|血管]]和[[神經系統|神經]]環繞在椎間盤的外面,並不會伸入椎間盤之中[15]。椎間盤裡面的細胞為特化的細胞,在不需要直接血液供應的狀態下亦能生存[15]。隨著年紀漸增,椎間盤會逐漸「退化」─失去彈性及吸收脊柱應力的能力[6],因而使脊柱整體的受力增加;此時,脊柱旁的韌帶會逐漸變厚、脊柱邊的骨頭會增生以因應脊柱受力增加的情況[6]。這些增厚增生的韌帶及骨頭會擠壓脊髓腔,使原本空間就很有限的脊髓腔,以及脊柱旁神經根通過的小孔[6],造成背痛的情形。在椎間盤退化的同時,血管及神經也可能會長入椎間盤之中[15],壓迫到神經根,導致背痛[15]。
疼痛感 Pain sensation
Pain is generally an unpleasant feeling in response to an event that either damages or can potentially damage the body’s tissues. There are four main steps in the process of feeling pain: transduction, transmission, perception, and modulation.[13] The nerve cells that detect pain have cell bodies located in the dorsal root ganglia and fibers that transmit these signals to the spinal cord.[16]The process of pain sensation starts when the pain-causing event triggers the endings of appropriate sensory nerve cells. This type of cell converts the event into an electrical signal by transduction. Several different types of nerve fibers carry out the transmission of the electrical signal from the transducing cell to the posterior horn of spinal cord, from there to the brain stem, and then from the brain stem to the various parts of the brain such as the thalamus and the limbic system. In the brain, the pain signals are processed and given context in the process of pain perception. Through modulation, the brain can modify the sending of further nerve impulses by decreasing or increasing the release of neurotransmitters.[13]
疼痛本質上是對於可能造成身體組織傷害的[[刺激]]所產生的反應。「感覺到疼痛」的過程包含了四個步驟:{{link-en|傳導|Transduction_(physiology)}}、傳遞、{{link-en|接收|Perception}}及{{link-en|調節|Neuromodulation}}[13]。能偵測疼痛的神經細胞其本體位在{{link-en|背根神經節|Posterior_root_ganglion}},並透過神經纖維將疼痛的訊息傳至脊髓[16]。「疼痛」起始於一個會引發疼痛的事件刺激了{{link-en|感覺神經的末梢|Nociceptor}},而感覺神經將刺激轉換為電訊號(稱作傳導,transduction)後傳遞至{{link-en|脊髓的後角|Posterior_grey_column}},經{{link-en|後角|Posterior_grey_column}}中的神經細胞轉接後傳遞[[腦幹]],接著被送至大腦各處,包括了[[丘腦]]及[[邊緣系統]]。當腦接受到疼痛的訊號後,會加以處理及「理解」,產生疼痛的感覺。大腦可以透過[[神经递质|神經傳導物質]]釋放的多寡來調節疼痛的狀況[13]。
Parts of the pain sensation and processing system may not function properly; creating the feeling of pain when no outside cause exists, signaling too much pain from a particular cause, or signaling pain from a normally non-painful event. Additionally, the pain modulation mechanisms may not function properly. These phenomena are involved in chronic pain.[13]
上述所提到的疼痛產生機制有時會失常─如沒有外在刺激仍然會產生疼痛的訊號、針對某刺激產生過量的疼痛訊號、針對原本不會引起疼痛的刺激卻產生疼痛訊號;此外,大腦的疼痛調節機制也有可能失常。這些狀況可能和慢性疼痛的產生有關[13]。
As the structure of the back is complex and the reporting of pain is subjective and affected by social factors, the diagnosis of low back pain is not straightforward.[8] While most low back pain is caused by muscle and joint problems, this cause must be separated from neurological problems, spinal tumors, fracture of the spine, and infections, among others.[1][17]
由於背部的解剖結構複雜,加上疼痛感本身有時相當[[主觀]]且受環境與社會因子影響,下背痛的診斷並不容易確立[8]。下背痛多半還是肌肉關節的問題所造成,這項成因必須和其他造成下背痛的原因─如神經系統的問題、脊椎腫瘤、脊椎骨折、脊椎的感染等等作鑑別[1][17]。
分類Classification
There are a number of ways to classify low back pain with no consensus that any one method is best.[8] There are three general types of low back pain by cause: mechanical back pain (including nonspecific musculoskeletal strains, herniated discs, compressed nerve roots, degenerative discs or joint disease, and broken vertebra), non-mechanical back pain (tumors, inflammatory conditions such as spondyloarthritis, and infections), and referred pain from internal organs (gallbladder disease, kidney stones, kidney infections, and aortic aneurysm, among others).[8] Mechanical or musculoskeletal problems underlie most cases (around 90% or more),[8][18] and of those, most (around 75%) do not have a specific cause identified, but are thought to be due to muscle strain or injury to ligaments.[8][18] Rarely, complaints of low back pain result from systemic or psychological problems, such as fibromyalgia and somatoform disorders.[18]
下背痛的分類有很多種,目前並沒有公認且統一的分類方式[8]。就成因而言,下背痛可被分成三大類:機械性的背痛(包括肌肉拉傷、[[椎间盘脱出症|椎間盤突出]]、{{link-en|脊神經根|Nerve_root}}被壓迫、{{link-en|椎間盤退化|Degenerative_disc_disease}}、[[骨关节炎|關節疾病]]、脊椎骨折等。)、非機械性的背痛([[腫瘤]]、發炎─如{{link-en|脊柱關節炎|Spondyloarthropathy}}、感染)、及來自內臟器官的{{link-en|轉移痛|Referred_pain}}(如{{link-en|來自膽囊|Biliary_colic}}、[[腎結石]]、{{link-en|腎臟感染|Pyelonephritis}}、{{link-en|主動脈瘤|Aortic aneurysm}}等內臟器官[8])。機械性的背痛佔了多數的病例(約略90%、或超過90%[8][18]),至於找不到原因的背痛有大部分(約75%)仍被認為是和肌肉拉傷、韌帶受傷有關[8][18]。少數的背痛可能是全身性的問題(如{{link-en|肌痛症|fibromyalgia}})或是精神方面的問題(如[[身心性疾病|身體化疾患]])所引起[18]。
Low back pain may be classified based on the signs and symptoms. Diffuse pain that does not change in response to particular movements, and is localized to the lower back without radiating beyond the buttocks, is classified as nonspecific, the most common classification.[8] Pain that radiates down the leg below the knee, is located on one side (in the case of disc herniation), or is on both sides (in spinal stenosis), and changes in severity in response to certain positions or maneuvers is radicular, making up 7% of cases.[8] Pain that is accompanied by red flags such as trauma, fever, a history of cancer or significant muscle weakness may indicate a more serious underlying problem and is classified as needing urgent or specialized attention.[8]
下背痛也可根據症狀及徵候來分類。
「’’非特異性’’」:其疼痛僅侷限在下背部,是最常見的類型。此類型不由特定動作引起,且未延伸至[[臀|臀部]][8]。
「’’脊神經根病變’’」:因脊神經根被壓迫而造成的疼痛,約占所有患者的7%。疼痛會延伸至腿部(多半至膝蓋以下),可能是單側疼痛(常見於椎間盤突出)或雙側疼痛(常見於脊椎腔狹窄),且特定姿勢可能會加重疼痛[8]。
「“其他類型”」:下背痛若伴隨其他外傷、發燒、嚴重肌無力或癌症病史,代表可能有較嚴重的潛在原因,這一類患者須緊急處理或特殊照護[8]。
The symptoms can also be classified by duration as acute, sub-chronic (also known as sub-acute), or chronic. The specific duration required to meet each of these is not universally agreed upon, but generally pain lasting less than six weeks is classified as acute, pain lasting six to twelve weeks is sub-chronic, and more than twelve weeks is chronic.[17]Management and prognosis may change based on the duration of symptoms.
另外,也可以用症狀持續的時間長短來分類,分為急性、亞急性及慢性。雖然沒有絕對的共識,但一般以六週及十二週為界,六週以內稱作急性、六到十二週稱為亞急性、十二週以上稱為慢性[17]。治療策略的選擇常和症狀持續的長短有很大的關聯。
危險徵象 Red flags
| 原文 | 翻譯 | 連結 | 原文 | 翻譯 | 連結 |
| Red flag[19] | 危險徵象[19] | 無 | Possible cause[1] | 可能原因[1] | 無 |
| Previous history of cancer | 過去曾患癌症 | 無 | Cancer | 癌症 | 無 |
| Unexplained weight loss | 原因不明的體重減輕 | 無 | Cancer | 癌症 | 無 |
| Loss of bladder or bowel control | 大小便失禁 | 無 | Cauda equina syndrome | 脊髓馬尾症候群 | https://en.wikipedia.org/wiki/Cauda_equina_syndrome |
| Significant motor weakness | 明顯運動無力或感覺障礙 | 無 | Cauda equina syndrome | 脊髓馬尾症候群 | 無 |
| Loss of sensation in the | 臀部感覺喪失(馬鞍區麻痺) | https://en.wikipedia.org/wiki/Saddle_anesthesia | Cauda equina syndrome | 脊髓馬尾症候群 | 無 |
| Significant trauma related to age | 發生對該年齡層而言嚴重的創傷[譯注2] | 無 | Fracture | 骨折 | 無 |
| Chronic corticosteroid use | 長期使用類固醇 | 無 | Fracture | 骨折 | 無 |
| Severe pain after lumbar | 過去腰椎曾接受手術的部位有疼痛的情形 | 無 | Infection | 感染 | 無 |
| Fever | 發燒 | 無 | Infection | 感染 | 無 |
| Urinary tract infection | 尿道感染 | 無 | Infection | 感染 | 無 |
| Immunosuppression | 免疫抑制 | https://en.wikipedia.org/wiki/Immunosuppression | Infection | 感染 | 無 |
| Intravenous drug use | 靜脈用藥 | 無 | Infection | 感染 | 無 |
Red flags are warning signs that may indicate a more serious problem
危險徵象的出現表示可能有更嚴重問題的警訊。
The presence of certain signs, termed red flags, indicate the need for further testing to look for more serious underlying problems, which may require immediate or specific treatment.[8] The presence of a red flag does not mean that there is a significant problem. It is only suggestive,[20][21] and most people with red flags have no serious underlying problem.[1][17] If no red flags are present, performing diagnostic imaging or laboratory testing in the first four weeks after the start of the symptoms has not been shown to be useful.[8]
所謂的「危險徵象」({{lang-en|[[:en:Red_flag#Science|red flags]]}}),指的是當有這些徵象出現時,最好能盡速就醫以尋找潛在的原因並接受相對應的醫療處理[8]。但這並不代表危險徵象出現時一定有嚴重的潛藏原因[20][21],事實上大部分有出現危險徵象的病人並沒有特別嚴重的潛在問題[1][17]。研究指出,若病人的背痛沒有伴隨危險徵象的出現,在症狀開始的四週內做[[醫學影像|影像]]或實驗室檢查並沒有助益[8]。
The usefulness of many red flags are poorly supported by evidence.[22] The most useful for detecting a fracture are: older age,corticosteroid use, and significant trauma especially if it results in skin markings.[22] The best determinate for the presence of cancer is a history of the same.[22]
目前研究認為這些「危險徵象」的出現,對於推斷背痛的原因是來自骨折或癌症並沒有太大幫助[22]。其中對於推斷背痛來自於骨折可能比較有用的因子包括:較大的年紀、使用[[皮質類固醇|類固醇]]、之前受到嚴重的創傷[22]。至於推斷背痛可能來自癌症最有用的因子則是病人本身有癌症的病史[22]。
With other causes ruled out, people with non-specific low back pain are typically treated symptomatically, without exact determination of the cause.[1][17] Efforts to uncover factors that might complicate the diagnosis, such as depression, substance abuse, or an agenda concerning insurance payments may be helpful.[8]
當常見造成背痛的原因都被排除後,背痛真正的成因通常無法完全找到,此時會先針對症狀給予治療[1][17]。此外,尋找一些如憂鬱、成癮性物質濫用、醫療保費申請等潛在的因子可能對找到造成背痛的真正原因有所幫助[8]。
檢查Tests

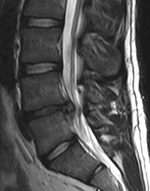
The straight leg raise test can detect pain originating from a herniated disc. When warranted, imaging such as MRI can provide clear detail about disc related causes of back pain (L4–L5 disc herniation shown)
在檢查下背痛的成因中,可以在患者躺平的情況下,將腿伸直並逐漸抬高,以是否會引發疼痛藉此判斷下背動的成因是否由椎間盤凸出所造成。而核磁共振顯影可以協助診斷並提供解剖學上的資訊。
{{double image|right|Straight-leg-test.gif|200|L4-l5-disc-herniation.png|150|在檢查下背痛的成因中,可以在患者躺平的情況下,將腿伸直並逐漸抬高,以是否會引發疼痛藉此判斷下背動的成因是否由椎間盤凸出所造成。而核磁共振顯影可以協助診斷並提供解剖學上的資訊。(圖中顯示為腰椎第4與第5節的椎間盤突出) }}
Imaging is indicated when there are red flags, ongoing neurological symptoms that do not resolve, or ongoing or worsening pain.[8] In particular, early use of imaging (either MRI or CT) is recommended for suspected cancer, infection, or cauda equina syndrome.[8] MRI is slightly better than CT for identifying disc disease; the two technologies are equally useful for diagnosing spinal stenosis.[8] Only a few physical diagnostic tests are helpful.[8] The straight leg raise test is almost always positive in those with disc herniation.[8] Lumbar provocative discography may be useful to identify a specific disc causing pain in those with chronic high levels of low back pain.[23] Similarly, therapeutic procedures such as nerve blocks can be used to determine a specific source of pain.[8] Some evidence supports the use of facet joint injections, transforminal epidural injections and sacroilliac injections as diagnostic tests.[8] Most other physical tests, such as evaluating for scoliosis, muscle weakness or wasting, and impaired reflexes, are of little use.[8]
當出現上述所提的危險徵象、持續的神經學症狀、持續或越來越嚴重的疼痛時,建議做影像學檢查[8],尤其是當懷疑是癌症、感染或{{link-en|脊髓馬尾症候群|cauda equina syndrome}}時,最好能盡早做電腦斷層或核磁共振等影像檢查[8]。核磁共振比起電腦斷層更能偵測到椎間盤的病變,但兩者對於檢查脊椎腔狹窄都很有用[8]。至於身體檢查方面,只有少數幾個檢查項目比較有用[8],其中「{{link-en|抬腳測試|straight leg raise test}}」在椎間盤突出時幾乎都會呈現陽性反應(病患腳被抬起時會覺得疼痛)。利用{{link-en|脊神經阻斷術|Lumbar_provocative_discography}}或可找到造成長期劇烈疼痛的椎間盤[23]。類似的概念如神經傳導阻斷療法也可以確認特定背痛的來源[8],有些證據顯示{{link-en|將麻醉藥注入小面關節/關節突間關節(facet joint)|Facet_joint_injection}}、薦髂關節(sacroiliac joint)以阻斷神經可能是有用的診斷方法[8]。
Complaints of low back pain are one of the most common reasons people visit doctors.[24][25] For pain that has lasted only a few weeks, the pain is likely to subside on its own.[26] Thus, if a person’s medical history and physical examination do not suggest a specific disease as the cause, medical societies advise against imaging tests such as X-rays, CT scans, and MRIs.[25] Individuals may want such tests but, unless red flags are present,[27][28] they are unnecessary health care.[24][26]Routine imaging increases costs, is associated with higher rates of surgery with no overall benefit,[29][30]and the radiation used may be harmful to one’s health.[29] Fewer than 1% of imaging tests identify the cause of the problem.[24] Imaging may also detect harmless abnormalities, encouraging people to request further unnecessary testing or to worry.[24] Even so, MRI scans of the lumbar region increased by more than 300% among United States Medicare beneficiaries from 1994 to 2006.[31]
背痛是病患求診最常見的原因[24][25]。幾周內的疼痛常會自己好[26],因此若沒有從病患的[[病史]]或[[体格检查|身體檢查]]之中找到特定背痛原因的話,一般不建議進一步做影像檢查,包括[[X射线|X光]]、[[X射线计算机断层成像|電腦斷層]]、[[核磁共振成像|核磁共振]][25]。很多病患會要求影像檢查,但除非有「危險徵象」[27][28],否則{{link-en|這些檢查並非必要|unnecessary health care|非必要之醫療服務}}[24][26]。常規做影像檢查除了會增加成本外,也會增加可能沒有益處的手術比率[29][30],且影像檢查帶來的輻射劑量對人體健康也有害處[29]。事實上,從影像檢查中找出背痛原因的比率小於1%[24],而影像也可能顯示出對健康沒有影響的異常,而這些異常即使無害,有時仍造成病人擔心甚至會要求接受進一步的治療[24]。即便如此,腰椎的核磁共振檢查總量從1994到2006年來成長了300%[31]。

[[File:Lifting Techniques.png|thumb|right|Lifting technique suggested to avoid low back pain]]
[[File:Lifting Techniques.png|thumb|right|避免發生下背痛的抬重物技巧]]。1. 臉正向前進的方向; 2. 良好的握姿; 3. 將脊椎維持直立的姿勢; 4. 雙腳與臀部同寬,並且以不平行的姿勢維持良好的穩定度
Effective methods to prevent low back pain have not been well developed.[32] Exercise is probably effective in preventing recurrences in those with pain that has lasted more than six weeks.[1][33] Medium-firm mattresses are more beneficial for chronic pain than firm mattresses.[34] There is little to no evidence that back belts are any more helpful in preventing low back pain than education about proper lifting techniques.[35] Shoe insoles do not help prevent low back pain.[36]
目前尚未有有效預防下背痛的方法[32]。對於背痛超過六周的病人,[[體能鍛鍊|運動]]可能有助於減少症狀的復發[1][33]。中等硬度的床墊相較於硬的床墊而言,對慢性背痛患者較佳[34]。所謂的「{{link-en|腰部支撐腰帶|Back belt}}」目前並沒有證據顯示其有效,可能還不如教導病人正確的搬起重物的姿勢與方式[35]。{{link-en|鞋墊|Shoe insert}}對預防背痛並無效果[36]。
Management of low back pain depends on which of the three general categories is the cause: mechanical problems, non-mechanical problems, or referred pain.[37] For acute pain that is causing only mild to moderate problems, the goals are to restore normal function, return the individual to work, and minimize pain. The condition is normally not serious, resolves without much being done, and recovery is helped by attempting to return to normal activities as soon as possible within the limits of pain.[17] Providing individuals with coping skills through reassurance of these facts is useful in speeding recovery.[1] For those with sub-chronic or chronic low back pain, multidisciplinary treatment programs may help.[38]
背痛的治療原則和背痛成因的三大分類(機械性背痛、非機械性背痛、轉移痛)有關[37]。針對症狀輕微到中等的急性背痛,治療目標在於恢復病患原本的正常功能、使病患能回到工作岡位、減少疼痛。這類的狀況一般不嚴重,常不需要太積極的治療也會自然緩解,在疼痛緩解後盡早恢復正常的活動有助於整體的康復[17]。告知患者關於下背痛的前述資訊,對於其心理上{{link-en|因應|Coping skills}}因應疼痛、加速康復,也會有幫助的效果。對於亞慢性或慢性疼痛的患者,給予複合性的訓練治療計劃也許會有所幫助[38]。
物理治療 Physical management
Increasing general physical activity has been recommended, but no clear relationship to pain or disability has been found when used for the treatment of an acute episode of pain.[33][39] For acute pain, low- to moderate-quality evidence supports walking.[40] Treatment according to McKenzie method is somewhat effective for recurrent acute low back pain, but its benefit in the short term does not appear significant.[1]There is tentative evidence to support the use of heat therapy for acute and sub-chronic low back pain[41] but little evidence for the use of either heat or cold therapy in chronic pain.[42] Weak evidence suggests that back belts might decrease the number of missed workdays, but there is nothing to suggest that they will help with the pain.[35] Ultrasound and shock wave therapies do not appear effective and therefore are not recommended.[43]
患者通常被建議增加日常活動,但沒有明顯的證據顯示可以改善急性疼痛發作時的疼痛及失能[33][39]。下背痛急性發作時,有部分的醫學研究顯示步行能夠有所幫助[40];而{{link-en|Mckenzie物理療法|McKenzie method}}對反覆的急性下背痛有點效果,但短期操作的療效則不顯著[1]。有初步證據顯示熱療對急性和亞慢性的下背痛的療效[41];但利用熱療或冷療治療慢性下背痛的效果,則沒有明顯定論[42]。僅有少量的證據顯示,使用護腰雖然能讓患者較快回到工作岡位上,但卻無助於緩解疼痛。[35]。超音波及衝擊波治療則沒有療效,因此通常不是建議的治療手法[43]。
Exercise therapy is effective in decreasing pain and improving function for those with chronic low back pain.[35] It also appears to reduce recurrence rates for as long as six months after the completion of program[44] and improves long-term function.[42] There is no evidence that one particular type of exercise therapy is more effective than another.[45] The Alexander technique appears useful for chronic back pain,[46]and there is tentative evidence to support the use of yoga.[47] Transcutaneous electrical nerve stimulation (TENS) has not been found to be effective in chronic low back pain.[48] Evidence for the use of shoe insoles as a treatment is inconclusive.[36] Peripheral nerve stimulation, a minimally-invasive procedure, may be useful in cases of chronic low back pain that do not respond to other measures, although the evidence supporting it is not conclusive, and it is not effective for pain that radiates into the leg.[49]
{{link-en|運動治療|Exercise therapy}}能有效的緩解慢性下背痛的疼痛,改善患者日常功能[35];此外,也可促進長期功能的改善[42],並減少療程結束後6個月內的再復發率 [44]。然而,並無證據顯示哪一種運動對於下背痛特別有效[45]。證據顯示[[亞歷山大技巧|Alexander法]]對慢性背痛有用[46],而初步的證據顯示,[[瑜伽]]也有效果[47]。{{link-en|經皮神經電刺激|Transcutaneous electrical nerve stimulation}}被認為對慢性下背痛沒有效果[48],使用鞋墊是否有幫助則尚無定論[36]。倘若慢性下背痛患者對上述療法的反應都不大,{{link-en|週邊神經刺激|Electroanalgesia}} (輕微的侵入性療法)或許能有所改善,但醫學效果不一。且已知此一療法並不能改善已經延伸至腿部的疼痛[49]。
藥物治療 Medications
The management of low back pain often includes medications for the duration that they are beneficial. With the first episode of low back pain the hope is a complete cure; however, if the problems becomes chronic, the goals may change to pain management and the recovery of as much function as possible. As pain medications are only somewhat effective, expectations regarding their benefit may differ from reality, and this can lead to decreased satisfaction.[4]
在利用藥物舒緩下背痛的治療方面來說,通常會針對不同階段的疼痛進程,使用不同的藥物。對於最初階段的下背痛,用藥的方針是希望完全治癒,然而一旦下背痛轉為慢性疼痛,用藥的目標就可能改為疼痛控制,以及盡可能地恢復患者的正常生活機能。由於止痛藥物只能達到部分層面效果,對於藥物助益的期待可能與現實有落差,這有可能造成患者滿意度的下降[4]。
The medication typically recommended first is acetaminophen or NSAIDs (though not aspirin), and these are enough for most people. Standard doses of acetaminophen are very safe; however, very high doses may cause liver problems.[4] NSAIDs are more effective for acute episodes than acetaminophen; however, they carry a greater risk of side effects including: kidney failure, stomach ulcers and possibly heart problems. Thus, NSAIDs are a second choice to acetaminophen, recommended only when the pain is not handled by the latter. NSAIDs are available in several different classes; there is no evidence to support the use of COX-2 inhibitors over any other class of NSAIDs with respect to benefits.[4] With respect to safety naproxen may be best.[50] Muscle relaxants may also be beneficial.[4]
通常第一線的建議用藥為[[對乙醯氨基酚]]({{lang-en|acetaminophen}})或[[非類固醇消炎止痛藥]]({{lang-en|NSAIDs}})(阿斯匹靈除外),而這對大部分的患者來說已經足夠了。標準劑量的對乙醯氨基酚非常安全,然而高劑量下可能造成{{link-en|肝臟毒性|Hepatotoxicity}}[4]。非類固醇消炎止痛藥對急性發作較對乙醯氨基酚更有效,但該類藥物也有更大的風險產生以下的副作用,可能的副作用包含[[腎功能衰竭]]、[[胃及十二指腸潰瘍]]以及[[心血管疾病]]。因此相較於對乙醯氨基酚而言,非類固醇消炎止痛藥是第二選項用藥,只有當對乙醯氨基酚無法有效控制下背痛時才推薦使用。沒有實質證據顯示環氧合酶抑制劑({{lang-en|COX-2 inhibitor}})較其他種類的非類固醇消炎止痛藥對疼痛更有助益。根據安全方面的考量[[萘普生]]({{lang-en| naproxen}})為首選[50]。[[肌肉鬆弛劑]]也可能有幫助[4]。
If the pain is still not managed adequately, opioids such as morphine may be used. These medications carry a risk of addiction, may have negative interactions with other drugs, and have a greater risk of side effects, including dizziness, nausea, and constipation. Opioids may be suitable for short-term management of severe, acute pain that is causing significant problems.[4] Specialist groups advise against general long-term use of opioids for chronic low back pain.[4] For older people with chronic pain, opioids may be used in those for whom NSAIDs present too great a risk, such as those with diabetes, stomach or heart problems. They may also be useful for a select group of people with neuropathic pain.[51]
若疼痛仍無法緩解,則可以考慮使用[[鴉片類藥物]](如[[嗎啡]])。鴉片類藥物可能有成癮的風險、與其他藥物的交互作用、以及副作用包括暈眩、嘔心、便秘等。鴉片類藥物可能適用於急性嚴重疼痛之短期處置[4],然而專家不建議長期使用於慢性下背痛[4]。對於老年人(如患有糖尿病、胃病、或心臟疾病)使用非類固醇消炎藥之風險較高時,可考慮使用鴉片類藥物。此外,對於{{link-en|神經痛|Neuropathic pain}}的病人,鴉片類藥物也可能有效[51]。
Antidepressants may be effective for treating chronic pain associated with symptoms of depression, but they have a risk of side effects. Although the antiseizure drugs gabapentinand carbamazepine are sometimes used for chronic low back pain and may relieve sciatic pain, there is insufficient evidence to support their use.[4]Systemic oral steroids have not been shown to be useful in low back pain.[1][4] Facet joint injections and steroid injections into the discs have not been found to be effective in those with persistent, non-radiating pain; however, they may be considered for those with persistent sciatic pain.[52] Epidural corticosteroid injections provide a slight and questionable short-term improvement in those with sciatica but are of no long term benefit.[53]
[[抗憂鬱劑|抗憂鬱藥]]也可能對治療與憂鬱症狀相關的慢性疼痛有幫助,但這類藥物具有副作用的風險。雖然抗癲癇藥物加巴噴丁({{lang-en| gabapentin}})、卡馬西平({{lang-en| carbamazepine}})有時會被用作治療慢性下背痛的藥物,而且可能可以減緩{{link-en|坐骨神經痛|Sciatica}},但未有充足的證據支持此說[4]。口服[[類固醇]]對於治療下背痛並沒有療效[1][4]。若直接注射類固醇於{{link-en|小面關節/關節突間關節|Zygapophysial_joint}}和椎間盤中,也許能對持續不斷的坐骨神經痛有所幫助,但卻對於持續地、非輻射狀的疼痛沒有幫助[52]。對有坐骨神經痛的患者而言,{{link-en|硬脊膜外的|Epidural}}注射類固醇,能夠輕微且短暫地減輕疼痛,但長期而言,並沒有幫助[53]。
手術治療 Surgery
Surgery may be useful in those with a herniated disc that is causing significant pain radiating into the leg, significant leg weakness, bladder problems, or loss of bowel control.[54] It may also be useful in those with spinal stenosis.[55] In the absence of these issues, there is no clear evidence of a benefit from surgery.[54]
對於那些由椎間盤突出所引起的腿部疼痛、明顯的腿部無力、膀胱問題、大便失禁等困擾,藉由手術的改善可能會有所助益[54]。手術對於治療{{link-en|脊椎狹窄症候群|Spinal stenosis}}也可能有效[55]。若非由上述原因引起的下背痛,目前並沒有明確的證據顯示手術對病人有實質助益[54]。
Discectomy (the partial removal of a disc that is causing leg pain) can provide pain relief sooner than nonsurgical treatments.[54] Discectomy has better outcomes at one year but not at four to ten years.[54] The less invasive microdiscectomy has not been shown to result in a different outcome than regular discectomy.[54]For most other conditions, there is not enough evidence to provide recommendations for surgical options.[54] The long-term effect surgery has on degenerative disc disease is not clear.[54] Less invasive surgical options have improved recovery times, but evidence regarding effectiveness is insufficient.[54]
{{link-en|椎間盤切除術|Discectomy}}(將造成腿部疼痛的椎間盤,進行該組織的局部切除)比其他非手術的治療法能夠更快地解除病人的疼痛[54]。但是手術只會在一年內會具有比較好的效果,延長至四到十年則沒有顯著的益處[54]。目前沒有證據顯示,微創式的椎間盤切除術與傳統的切除術兩者之間的療效有所差異[54]。對大多數其他的情況,都沒有足夠的證據可以做為支持患者接受手術治療的依據[54]。對於退化性椎間盤引起的下背痛,手術治療的長期影響並不明確[54]。微創手術可以縮短復原的時間,但沒有足夠的證據顯示對於患者的幫助更大[54]。
For those with pain localized to the lower back due to disc degeneration, fair evidence supports spinal fusion as equal to intensive physical therapy and slightly better than low-intensity nonsurgical measures.[55]
而因為退化性椎間盤引起的下背痛,目前的醫學證據顯示,加強的物理療法以及{{link-en|脊柱固合術|Spinal fusion}}顯示了相同的療效,且效果優於低強度的非手術療法[55]。
Fusion may be considered for those with low back pain from acquired displaced vertebra that does not improve with conservative treatment,[54]although only a few of those who have spinal fusion experience good results.[55] There are a number of different surgical procedures to achieve fusion, with no clear evidence of one being better than the others.[56] Adding spinal implant devices during fusion increases the risks but provides no added improvement in pain or function.[31]
對於脊柱錯位(或者{{link-en|脊椎滑脫|Spondylolisthesis}})而引起的下背痛患者,若無法藉由保守治療獲得症狀的改善,脊柱固合術則可能考慮被採用[54]。僅管通常只有少數的患者能在接受手術後獲得好的療效[55]。執行脊柱固合術的手術方式有好幾種,但目前沒有沒有證據顯示那一種是最好的[56]。執行固合術時加入植入式植體會增加手術風險,且對於疼痛或功能的改善沒有幫助[31]。
整合輔助治療 Alternative medicine
It is not clear if chiropractic care or spinal manipulation therapy (SMT) improves outcomes in those with low back pain more or less than other treatments.[57] Some reviews find that SMT results in equal or better improvements in pain and function when compared with other commonly used interventions for short, intermediate, and long-term follow-up;[58][59]other reviews find it to be no more effective in reducing pain than either inert interventions, sham manipulation, or other treatments, and conclude that adding SMT to other treatments does improve outcomes.[5][60] National guidelines reach different conclusions, with some not recommending spinal manipulation, some describing manipulation as optional, and others recommending a short course for those who do not improve with other treatments.[17] Manipulation under anaesthesia, or medically assisted manipulation, has not enough evidence to make any confident recommendation.[61]
使用 [[脊骨神經醫學]]或{{link-en|脊椎鬆動術|Spinal manipulation}}治療下背痛症狀的療效是否優於其他治療方式,目前未有定論[57]。某些文獻回顧發現在短期、中程、或長期的個案追蹤結果指出,脊椎鬆動術對於疼痛及功能的療效相當於其他常用的治療,或者效果更好[58][59]。其他文獻回顧指出脊椎鬆動術與其他保守治療及假性鬆動術(不正確或無效的鬆動手法)或其他治療相比,並不特別有效,但將脊椎鬆動術和其他治療項目一起治療則有助於整體療效[5][60]。國家指定治療方針(此處應指美國的醫療指示)導向不同的結論,有些不建議使用脊椎鬆動手法,有些則建議選用,而也有建議對於其他療法效果不彰的患者,可以接受短期的脊椎鬆動術做為治療項目[17]。{{link-en|麻醉後執行|Manipulation under anesthesia}}的鬆動手法,或在有其他醫療儀器協助下操作的鬆動術,並未有足夠的證據支持其成為必定有效的治療項目[61]。
Acupuncture is no better than placebo, usual care, or sham acupuncture for nonspecific acute pain or sub-chronic pain.[62] For those with chronic pain, it improves pain a little more than no treatment and about the same as medications, but it does not help with disability.[62] This pain benefit is only present right after treatment and not at follow-up.[62]Acupuncture may be a reasonable method to try for those with chronic pain that does not respond to other treatments like conservative care and medications.[1][63] While massage therapy does not appear to provide much benefit for acute low back pain,[1] it may help those with sub-chronic and chronic pain, particularly when combined with physical exercises and education.[64] Tentative evidence suggests that acupuncture and massage together may be better than massage alone.[64]
對非特定性急性疼痛者或亞慢性疼痛者而言,比起安慰劑、常規護理或{{link-en|安慰性|Sham surgery}}針灸,實際針灸的效果並不會更好[62]。對於慢性疼痛患者而言,接受針灸治療的組別,其疼痛改善的效果大於無治療的組別,並就改善疼痛的效果而言,接受針灸的患者與接受藥物治療的組別其療效相近;不過針灸對於失能者沒有幫助[62]。這種疼痛改善的效果只展現在剛治療完的時候,而非其預後[62]。對於慢性疼痛者而言,若保守治療或藥物治療沒有效果,針灸可能是個較可嘗試的選項[1][63]。[[按摩]]療法似乎對急性下背痛者沒有太大助益[1],但對亞慢性疼痛者與慢性疼痛者可能有幫助,尤其是結合身體鍛鍊與教育時較為顯著[64]。試驗證明,針灸搭配[[按摩]]療法會比單只有[[按摩]]療法更有助益。
Prolotherapy – the practice of injecting solutions into the joints of the back to cause inflammation and thereby stimulate the body’s healing response – has not been found to be effective by itself, although it may be helpful when added to another therapy.[5] Neuroreflexotherapy, in which small pieces of metal are placed just under the skin of the ear and back, appears to be effective in reducing low back pain and improving function, although the amount of evidence to support this is limited.[5][65] The herbal treatments Devil’s claw and white willow may reduce the number of individuals reporting high levels of pain; however, for those taking pain relievers, this difference is not significant.[5] Capsicum – in the form of either a gel or a plaster cast –has been found to reduce pain and increase function.[5]
{{link-en|增生療法|Prolotherapy}}:注入溶液到背部關節以引起發炎,從而刺激人體的癒合反應。沒有發現此療法有效果,但搭配其他療法或許有幫助[5]。
{{link-en|神經反射療法|Neuroreflexotherapy}}:將幾塊小金屬片放在耳朵或背部的皮膚下,看來似乎對於減緩下背痛、增進肢體功能有所幫助,但也有不少證據顯示,此療法的效果有限[5][65]。
草藥:{{link-en|南非鈎麻|Harpagophytum}}和[[白柳]]葉,似乎對於不少人減緩高強度的疼痛有效,但與使用止痛藥的效果無顯著差異[5]。
[[辣椒属|辣椒]]:以藥膏或藥布的形式使用,對於減緩疼痛和增進功能略有助益[5]。
Behavioral therapy may be useful for chronic pain.[66] There are several types available, including operant conditioning, which uses reinforcement to reduce undesirable behaviors and increase desirable behaviors; cognitive behavioral therapy, which helps people identify and correct negative thinking and behavior; and respondent conditioning, which can modify an individual’s physiological response to pain. Medical providers may develop an integrated program of behavioral therapies.[5] The evidence is inconclusive as to whether mindfulness-based stress reduction reduces chronic back pain intensity or associated disability, although it suggests that it may be useful in improving the acceptance of existing pain.[67]
[[行為治療]]也許對慢性疼痛有幫助[66]。目前有許多不同的方法:像是藉由減少不必要的動作、增加必要的動作,達成[[操作制約|操控制約]];[[認知行為療法|認知行為治療]]幫助患者辨識與矯正負面思考和負面行為;[[古典制約]]能夠修正患者對於痛覺的生理反應。醫療人員應該給予整合性的行為治療課程[5]。{{link-en|正念減壓課程|Mindfulness-based stress reduction}}是否能降低慢性背痛的強度,或緩解相關失能尚無結論,但似乎對於接受已經存在的痛覺有所幫助[67]。
Overall, the outcome for acute low back pain is positive. Pain and disability usually improve a great deal in the first six weeks, with complete recovery reported by 40 to 90%.[68] In those who still have symptoms after six weeks, improvement is generally slower with only small gains up to one year. At one year, pain and disability levels are low to minimal in most people. Distress, previous low back pain, and job satisfaction are predictors of long-term outcome after an episode of acute pain.[68] Certain psychological problems such as depression, or unhappiness due to loss of employment may prolong the episode of low back pain.[4] Following a first episode of back pain, recurrences occur in more than half of people.[2]
總體來說,急性下背痛的預後成果是正向的。在治療開始的6週內,通常在疼痛與功能障礙上會出現大幅度進展,據報告顯示,可以恢復到40-90%[68]。而在6週以後,通常進展開始變慢,直到治療後1年,才能達到小幅度成效。在治療後1年,大部分病患對於下背痛的疼痛與功能障礙,可以降至最低水平。痛苦程度、下背痛的發作歷史以及工作滿意度,是一段時期下背痛長期預後的預測指標[68]。特定的心理問題,如因失去工作而導致的憂鬱症或不快樂,可能會延長下背痛的預後時程[4]。一旦下背痛首次發生,約有一半的人會出現復發的可能[2]。
For persistent low back pain, the short-term outcome is also positive, with improvement in the first six weeks but very little improvement after that. At one year, those with chronic low back pain usually continue to have moderate pain and disability.[68] People at higher risk of long-term disability include those with poor coping skills or with fear of activity (2.5 times more likely to have poor outcomes at one year),[69] those with a poor ability to cope with pain, functional impairments, poor general health, or a significant psychiatric or psychological component to the pain (Waddell’s signs).[69]
對於持續性下背痛,短期的治療成效也是正向的。與急性相同的是,在治療開始的6週內有大幅度進展,但之後只有小幅度進展。在治療後1年,慢性下背痛病患通常仍會有中等程度的疼痛與功能障礙[68]。對於因應技能較差、害怕活動(一年大約是增加2.5倍的危險性)、克服疼痛的能力較差、功能性障礙、整體健康較差或是其疼痛與心理或精神因素相關({{link-en|非器質性症狀|Waddell’s signs}})的患者,有較高的危險性會變為長期功能障礙[69]。
Low back pain that lasts at least one day and limits activity is a common complaint.[32] Globally, about 40% of people have LBP at some point in their lives,[32] with estimates as high as 80% of people in the developed world.[70] Approximately 9 to 12% of people (632 million) have LBP at any given point in time, and nearly one quarter (23.2%) report having it at some point over any one-month period.[32][71]Difficulty most often begins between 20 and 40 years of age.[1] Low back pain is more common among people aged 40–80 years, with the overall number of individuals affected expected to increase as the population ages.[32]
持續時間超過一天的下背痛與活動受限,是常見的主訴症狀[32]。全球大約有四成的人,在一生當中曾經歷過下背痛[32],在已開發國家更高達八成[70]。將近9到12%的民眾(六億三千兩百萬人)時常都感到下背痛,有將近四分之一的民眾(23.2%)在某些時候的下背痛,持續至少有一個月之久[32][71]。多數病患在20到40歲時開始,對於下背痛感到困擾[1]。下背痛在40到80歲之間的民眾更為常見,當人口老化,受影響的人數將可預期的增加[32]。
It is not clear whether men or women have higher rates of low back pain.[32][71] A 2012 review reported a rate of 9.6% among males and 8.7% among females.[71] Another 2012 review found a higher rate in females than males, which the reviewers felt was possibly due to greater rates of pains due to osteoporosis, menstruation, and pregnancy among women, or possibly because women were more willing to report pain than men.[32]
下背痛在男性與女性的比例何者較高,目前仍不清楚[32][71]。在2012年的一篇文獻回顧,曾報告在男性與女性的比例分別為9.6%與8.7%[71]。另一篇同一年的文獻回顧則顯示在女性比例較高,而原因可能為女性骨質疏鬆、月經、懷孕等問題,或女性比男性更願意表達疼痛[32]。
An estimated 70% of women experience back pain during pregnancy with the rate being higher the further along in pregnancy.[72] Current smokers – and especially those who are adolescents – are more likely to have low back pain than former smokers, and former smokers are more likely to have low back pain than those who have never smoked.[73]
大約70%的女性曾有懷孕期間下背痛的經歷,而實際比例可能更高[72]。吸菸者,尤其青少年,比起戒菸者更可能有下背痛,而戒菸者又比不曾吸煙者較可能有下背痛[73]。
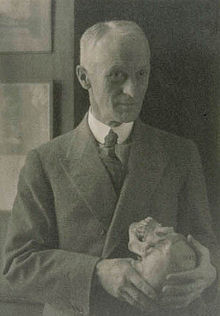
[[File:Harvey Cushing, Doris Ulmann 1920s.jpg|thumb|right|Harvey Williams Cushing, 1920s]]
[[File:Harvey_Cushing,_Doris_Ulmann_1920s.jpg|thumb|right|哈維·威廉斯·庫欣,攝於1920年代]]
Low back pain has been with humans since at least the Bronze Age. The oldest known surgical treatise – the Edwin Smith Papyrus, dating to about 1500 BCE – describes a diagnostic test and treatment for a vertebral sprain. Hippocrates (c. 460 BCE – c. 370 BCE) was the first to use a term for sciatic pain and low back pain; Galen (active mid to late second century CE) described the concept in some detail. Physicians through the end of the first millennium did not attempt back surgery and recommended watchful waiting. Through the Medieval period, folk medicine practitioners provided treatments for back pain based on the belief that it was caused by spirits.[74]
下背痛至少從[[青銅器時代]]就開始困擾人類。目前所知最早的外科專著「[[艾德溫·史密斯紙草文稿]]」(約可上溯至西元前1500年)中,描述了一次對脊椎扭傷的診斷測試和治療。[[希波克拉底]](約公元前460年-前370年)首先採用術語來稱呼坐骨神經痛和下背痛;[[蓋倫]](活躍於公元二世紀中晚期)透過一些細節描述了這個概念。在第一個千禧年結束之前,還沒有醫生嘗試過背部手術,而是建議{{link-en|觀察性等待|Watchful waiting|}}。直到[[中世紀]],民間醫學相信下背痛是由精神所引起,並以此為基礎進行治療[74]。
At the start of the 20th century, physicians thought low back pain was caused by inflammation of or damage to the nerves,[74] with neuralgia and neuritis frequently mentioned by them in the medical literature of the time.[75] The popularity of such proposed causes decreased during the 20th century.[75] In the early 20th century, American neurosurgeon Harvey Williams Cushing increased the acceptance of surgical treatments for low back pain.[54] In the 1920s and 1930s, new theories of the cause arose, with physicians proposing a combination of nervous system and psychological disorders such as nerve weakness (neurasthenia) and female hysteria.[74] Muscular rheumatism (now calledfibromyalgia) was also cited with increasing frequency.[75]
20世紀開始時,醫界認為下背痛是源自發炎或神經損傷[74],當時的醫學文獻中,經常跟神經痛或神經炎列在一起。在20世紀初期,下背痛的成因眾說紛紜,而在20世紀中期後,下背痛的成因眾說紛紜,而在20世紀中期後,因為椎間盤導致下背痛的理論逐漸成了主流[75]。20世紀早期,美國的神經外科醫師{{link-en|哈維·威廉斯·庫欣|Harvey Williams Cushing}}增加了採用外科手術治療下背痛的次數[54]。1920和1930年代,醫界提出了像神經耗弱({{link-en|神經衰弱症|neurasthenia}})和{{link-en|女性歇斯底里|female hysteria}}這類,神經系統和心理病病併發症的情形,下背痛病因的新理論也隨之出現[74]。肌風濕痛(現在稱為{{link-en|纖維肌痛|fibromyalgia}})被提及的次數也越來越多[75]。
Emerging technologies such as X-rays gave physicians new diagnostic tools, revealing the intervertebral disc as a source for back pain in some cases. In 1938, orthopedic surgeon Joseph S. Barr reported on cases of disc-related sciatica improved or cured with back surgery.[75] As a result of this work, in the 1940s, the vertebral disc model of low back pain took over,[74] dominating the literature through the 1980s, aiding further by the rise of new imaging technologies such as CT and MRI.[75] The discussion subsided as research showed disc problems to be a relatively uncommon cause of the pain. Since then, physicians have come to realize that it is unlikely that a specific cause for low back pain can be identified in many cases and question the need to find one at all as most of the time symptoms resolve within 6 to 12 weeks regardless of treatment.[74]
新興技術例如{{en-link|X光線照相術|Radiography|X光}},給了醫生們新的診斷工具,發現到椎間盤可能是某些病例中,導致下背痛的根源。1938年,整形外科醫生約瑟夫 S 巴爾提出一系列椎間盤相關坐骨神經病的病例,透過背部手術而獲得改善或治癒的報告[75]。因為這筆研究成果,在1940年代,用椎間盤模式解釋下背痛全盤接手[74],稱霸所有文獻直到1980年代,並且因為新的成像技術如[[電腦斷層掃描]](CT)和[[核磁共振成像]](MRI)得到更多的支持。
Low back pain results in large economic costs. In the United States, it is the most common type of pain in adults, responsible for a large number of missed work days, and is the most common musculoskeletal complaint seen in the emergency department.[6] In 1998, it was estimated to be responsible for $90 billion in annual health care costs, with 5% of individuals incurring most (75%) of the costs.[6] Between 1990 and 2001 there was a more than twofold increase in spinal fusion surgeries in the US, despite the fact that there were no changes to the indications for surgery or new evidence of greater usefulness.[31] Further costs occur in the form of lost income and productivity, with low back pain responsible for 40% of all missed work days in the United States.[76] Low back pain causes disability in a larger percentage of the workforce in Canada, Great Britain, the Netherlands and Sweden than in the US or Germany.[76]
下背痛導致大量經濟成本支出。這是在美國成人間最常見的疼痛,許多人因而請病假,甚至是在急診室中最常見的肌肉骨骼相關主訴[6]。根據預估,在1998年時,將近九百億的年度醫療照護預算可歸因於下背痛,其中有百分之五的患者使用了此預算中的百分之七十五[6]。在1999到2001年之間,儘管當時沒有修改脊椎融合手術的適應症或增加更多的用途,在美國的手術量卻有將近兩倍的成長[31]。失去收入和生產力帶來另一種層次的成本支出,在美國有四成的病假是因為下背痛所造成[76]。相較於美國和德國,下背痛在加拿大、英國、荷蘭與瑞典,造成大量勞動人力的功能障礙[76]。
Total disc replacement is an experimental option,[15] but no significant evidence supports its use over lumbar fusion.[54] Researchers are investigating the possibility of growing new intervertebral structures through the use of injected human growth factors, implanted substances, cell therapy, and tissue engineering.[15]
全椎間盤置換術現在仍被實驗研究中[15],但沒有顯著證據支持能被使用在腰椎固合的治療上[54]。研究人員正在研究利用注射人類生長因子、植入物、細胞療法和組織工程等方式,培養新的椎間組織以供患者使用[15]。
{{reflist|2}}